Dry Eye
Information Center
Answering your questions about Dry Eye
What is Dry Eye ?
The Signs and Symptoms
Recent studies suggest up to 30 million American’s have signs and symptoms of Ocular Surface Disease (OSD). In a day and age of constant computer and phone use, dry eye is more an epidemic today than ever before. Symptoms of dryness and ocular disease include:
- Burning, stinging sensation
- Fluctuations in vision with blinks
- Tired, fatigued eyes
- Red, irritated-looking eyes
- Excess tearing
- Inability to wear contact lenses
Many of our lives revolve around computer use. Many of us spend 12+ hours on the computer. Have you ever sat back and looked at the time and thought, “Wow, 3 hours just went by and I haven’t looked away from the screen. I don’t think I even blinked!”. Countless studies have shown that we blink 60% less while working on digital devices. Our ocular surface constantly needs to be refreshed with the spreading of new tears across the eye, so that is reduced by 60%. You can tell this is the case when you have to rub your eyes to get rid of that uncomfortable dry feeling.
Many other issues in our lives can lead to an increase in the signs and symptoms of dry eye.
Drugs considered to cause and aggravate OSD:
- Acne medication
- Antihistamines
- Anti-anxiety medications
- Birth Control
- Depression medication
- Eye drops
- Hormone Replacement
Other conditions that can increase and aggravate OSD:
- Diabetes
- Thyroid Disorders
- Auto-immune disorders (Sjogrens, Rheumatoid Arthritis, Lupus)
- Contact lens wear
- Sleep apnea
- Poor eyelid closure at night
- Previous eye surgery: Cataract, LASIK
Think that you might have Dry Eye?
Take two minutes to fill out the Ocular Surface Disease Index (OSDI) survey below. There is also a printable .pdf of this form here.
What is a Dry Eye Evaluation ?
Meibomian Glands Evaluation
Current research suggests that 85% of patients struggling with dry eye have a meibomian gland dysfunction. In a normal, healthy eye, the meibomian glands produce meibum, a substance similar to the color and consistency of generic vegetable oil. With each blink, a small amount of this oil is expressed from the meibomian glands and onto the ocular surface. The upper eyelid then pulls that oil over the surface of the eye. The purpose of this oil is to prevent evaporation of the tears, to create a smooth ocular surface resulting in clear consistent vision, and to decrease friction between the ocular surface and the upper eyelid.
Oil Evaluation
In Meibomian Gland Dysfunction (MGD), the oil is thick, almost like toothpaste, and can clog the glands. This results in little to no oil being expressed upon blinking. The tears on the eye evaporate quickly, causing a gritty, dry sensation, and difficulty staying comfortable in contact lenses. As part of the meibomian gland evaluation, it is necessary to evaluate the type of oil that is expressed.
Grade Scale for Meibomian Gland Dysfunction
Meibomian gland dysfunction is usually graded using the following scale. This system of grading helps the optometrist get a fuller picture of your dry eye symptoms, informing their decisions about what treatment options may be right for you.
| Grade Scale | Percentage of Blocked Glands | Quality of Meibomian Secretion |
|---|---|---|
| Grade 1 | 40%-50% | Clear to mild milky secretion |
| Grade 2 | 50%-70% | Milky to pasty secretion |
| Grade 3 | 70%-85% | Thick, pasty to very little secretion |
| Grade 4 | 85%-90% | Very little to no secretion |
Chronic blockage results in atrophy, or degeneration, of the glands. Unfortunately, gland atrophy is permanent damage. Once you lose the glands, you cannot get them back, so it’s vital to catch meibomian gland atrophy before the damage progresses too far.
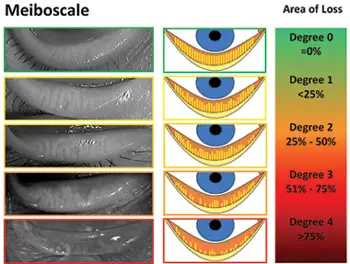
Degrees of Meibomian Gland Atrophy
The picture in the middle of the chart below is a great place to start the discussion of atrophy. The top picture (Degree 0 loss) is a healthy eye. The long yellow lines are the glands and the orange is the space between the glands. All the glands extend from the base of the lid to the lid margin. As you move down the scale (jump to Degree 4), you can see that the yellow lines are just stubs in comparison to Degree 0). Patients at grade 4 atrophy tend to be very uncomfortable, with chronic red, and irritated painful eyes. The pictures in the left hand column are the infrared photos of the real anatomy in dry eye patients. The sooner we discover the problem here, the more proactive we can be at slowing down this process.

Conjunctival Staining
Staining of the conjunctiva with dyes like Lissamine Green and Rose Bengal allows us to visualize dead and devitalized cells on the ocular surface. Any cells that are either dead or dying will absorb the dye. The amount of staining we see is then used to grade the degree of ocular disease.
Chronic blockage results in atrophy, or degeneration, of the glands. Unfortunately, gland atrophy is permanent damage. Once you lose the glands, you cannot get them back, so it’s vital to catch meibomian gland atrophy before the damage progresses too far.
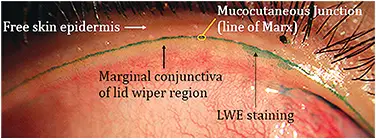
Lid Wiper Epitheliopathy
Lid Wiper Epitheliopathy can be evaluated using the same Lissamine Green dye seen above. Lid Wiper Epitheliopathy is a condition that occurs due to ocular trauma and friction between the upper lid and the ocular surface. This staining can present in a number of ways:
- Feather-like pattern: Stains that start vertically from the edge of the lid in the narrow brushstroke shape and variable length.
- Band pattern: This most common type of stain adopts a uniform band shape from the nasal to the temporal side of the inner eyelid margin. It often thickens at the center and then slightly thins towards the edges.
- Irregular pattern: Stains without any defined shape
Aqueous Evaluation
The aqueous, or water portion of the tears, is found between the mucin layer on the surface of the eye and the lipid layer, provided by the meibum from the meibomian glands. Aqueous is produced by the lacrimal gland up by the temple on the head, and drains through the punctum (inner tearduct). Research suggests that only a small percent of people have aqueous deficiency alone without a evaporative component (MGD). Since it can occur, however, we regularly monitor for it.
Ocular Environment
While often overlooked, the lashes and skin around the eyes also needs to be assessed. Oily skin, excessive makeup use, eczema, rosacea, and excessive bacteria can all combine to create a toxic environment, resulting in decreased tear production and increased inflammation. Proper lid hygiene is paramount in making sure that the meibomian glands are able to produce quality meibum and thrive.
Demodex
Demodex is a particular protozoa (think of a bug similar to bacteria) that lives on the eyelid and skin area. While bacteria on our skin is normal, this particular bug is not, and excessive amount leads to increased symptoms of dry eye. The reason is that Demodex digests skin cells, and also feeds on the meibum in the meibomian glands. Whats worse is they then procreate and lay eggs in the hair follicles of the eyelashes. This results in more demodex, and an increase in symptoms. Excessive amounts of demodex leads to:
- Color changes in the skin (Rosacea)
- Scaly Skin
- Red skin
- Sensitive or irritated skin
- Itching
- Rash
- Eye irritation
- Thickening of the eyelid
- Loss of eyelashes
This inflammation results in blepharitis. While blepharitis can manifest from a number of bacteria as well, demodex is significantly more aggressive and problematic. If you have dry eye symptoms, the likelihood of you having demodex is very high. Recent research has even noted up to 80% of individuals over the age of 60 have excessive amounts of demodex. Luckily, there are some very simply inexpensive treatments for demodex that often result in eradication of the mites if performed regularly. If you feel you might have demodex, schedule an appointment with Dr. Ward.

Schedule your Evaluation
Find Relief
Contact Us
Call us, email us, or visit our office and ask about setting up a Dry Eye Evaluation with Dr. Ward.
Get Evaluated
See Dr. Ward at our clinic where he will conduct a thorough evaluation of your dry eyes and help determine the best treatment options for YOU.
Get Treatment
Begin your treatments in whatever form they take and move one step closer to finding dry eye relief in your day-to-day life.


